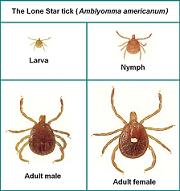
Tick species that transmit ehrlichiosis: Lone Star tick (Amblyomma americanum)
What is Ehrlichiosis?
Human Monocytic Ehrlichiosis (HME) , is caused by Ehrlichia chaffeensis, a type of bacteria known as rickettsia, and is transmitted to humans by the bite of the lone star tick Amblyomma americanum.
Unlike Lyme disease, ehrlichiosis is considered an acute infection without chronic long-term consequences. Its severity varies from person to person. Many people exposed to the disease agent exhibit no symptoms, while others suffer mild symptoms that resolve without treatment. In a minority of cases, however, ehrlichiosis produces severe symptoms requiring immediate antibiotic treatment. These cases can be life-threatening and even fatal for elderly patients and others with compromised immune systems.
Where is Ehrlichiosis Prevalent?
First identified in 1987, the HME bacterium E. chaffeensis is transmitted by the lone star tick. Ticks infected with E. chaffeensis occur mostly south of the line connecting southern New Jersey and western Texas, and throughout the high plains states north of Texas to the Canadian border. Recent expansion of the lone star tick into New York state (particularly Long Island) and coastal New England has resulted in cases of HME being reported from these areas with increased frequency.

Adult female Lone Star tick
Symptoms
Clinical manifestations of HME can range from mild to life-threatening depending on the patient’s age and general health.
Onset of ehrlichiosis generally begins within a week of a tick bite, and often includes fever, severe headaches, malaise, muscle pains, and chills. Other symptoms may include nausea, vomiting, confusion and joint pain. A rash may appear in some HME cases but unlike Lyme disease, this rash is general in nature and is not associated with the site of the tick bite.
Diagnosis
An initial diagnosis is based on the patient’s symptoms and laboratory tests. Routine laboratory results include a low white blood cell count, low platelet count and elevated liver enzymes (ALT, AST, LDH). A confirmed diagnosis can be made using an antibody IFA (Immuno-Fluorescent Assay) after 21 days of suspected infection. In severe cases, blood smears can be examined for ehrlichiosis.
Treatment
According to the Centers for Disease Control and Prevention (CDC), patients suspected of having ehrlichiosis should be treated immediately. Treatment should not be delayed until laboratory test results come back. Doxycycline is the drug of choice for ehrlichiosis patients. The CDC recommends 100 mg twice daily for adults or 4.4 mg/kg body weight per day in two divided doses for children under 100 lbs. Tetracycline can be used as an alternative if the patient is not pregnant (it is contraindiated for pregnant women). An alternative treatment for pregnant women is rifampin. The patient should continue to be treated at least three days after the fever subsides. Some physicians may treat for up to 28 days if the patient lives in an area endemic to Lyme disease on the chance that both disease agents have been transmitted. Ehrlichiosis symptoms usually subside within 24-48 hours of treatment; if not, the physician should consider other diagnoses.